2021 was the year the COVID-19 vaccines had to prove their mettle. We started the year full of hope: With vaccines in hand in record-breaking time and their rollout ramping up, we’d get shots in arms, curb this pandemic and get life back to normal. That was too optimistic.
Roughly 200 million people in the United States — and billions globally — have now been fully vaccinated. Three vaccines — one from Pfizer and its partner BioNTech, and the other two from Moderna and Johnson & Johnson — are available in the United States. Pfizer’s is even available for children as young as 5. About two dozen other vaccines have also been deployed in other parts of the world. In some higher-income countries, the United States included, people have already queued up for booster shots.
But 2021 has also been the year of learning the limits of the vaccines’ superpowers. With the vaccines pitted against aggressive coronavirus variants, inequitable distribution, some people’s hesitancy and the natural course of waning effectiveness, there’s still a lot of work to do to bring this pandemic to an end. As if to hammer home that point, the detection of the omicron variant in late November brought new uncertainty to the pandemic’s trajectory. Here are some of the top lessons we’ve learned in the first year of the COVID-19 vaccine. — Macon Morehouse
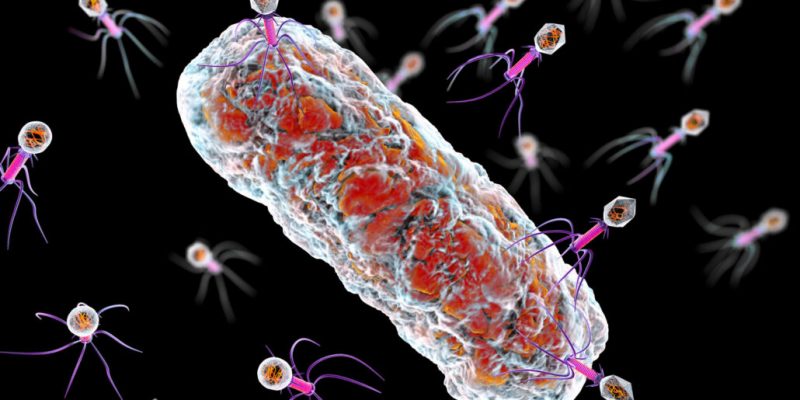
The shots work, even against emerging variants
Many COVID-19 vaccines proved effective over the last year, particularly at preventing severe disease and death (SN: 10/9/21 & 10/23/21, p. 4). That’s true even with the emergence of more transmissible coronavirus variants.
In January, in the midst of a bleak winter surge that saw average daily cases in the United States peaking at nearly 250,000, the vaccination rollout here began in earnest. Soon after, case numbers began a steep decline.
Over the summer, though, more reports of coronavirus infections in vaccinated people began to pop up. Protection against infection becomes less robust in the months following vaccination in people who received Pfizer’s or Moderna’s mRNA vaccines, multiple studies have shown (SN Online: 9/21/21). Yet the shots’ original target — preventing hospitalization — has held steady, with an efficacy of about 80 percent to 95 percent.
A single dose of Johnson & Johnson’s vaccine is less effective at preventing symptoms or keeping people out of the hospital than the mRNA jabs. The company claims there’s not yet evidence that the protection wanes. But even if that protection is not waning, some real-world data hint that the shot may not be as effective as clinical trials suggested (SN Online: 10/19/21).
Evidence of waning or lower protection ultimately pushed the United States and some other countries to green-light COVID-19 booster shots for adults (SN: 12/4/21, p. 6).
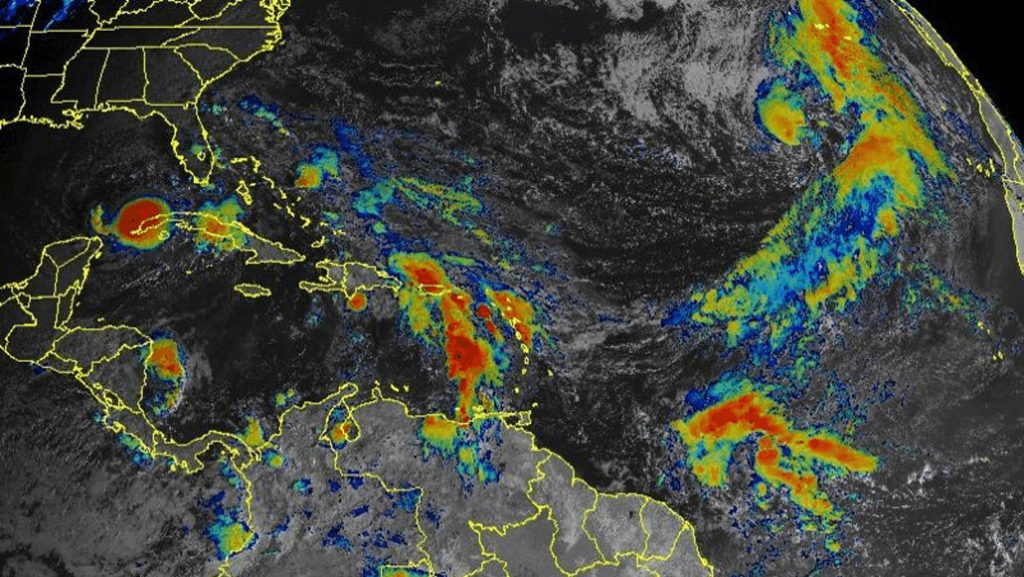
Much of the worry over waning immunity came amid the spread of highly contagious variants, including alpha, first identified in the United Kingdom in September 2020, and delta, first detected in India in October 2020 (SN Online: 7/30/21). Today, delta is the predominant variant globally.
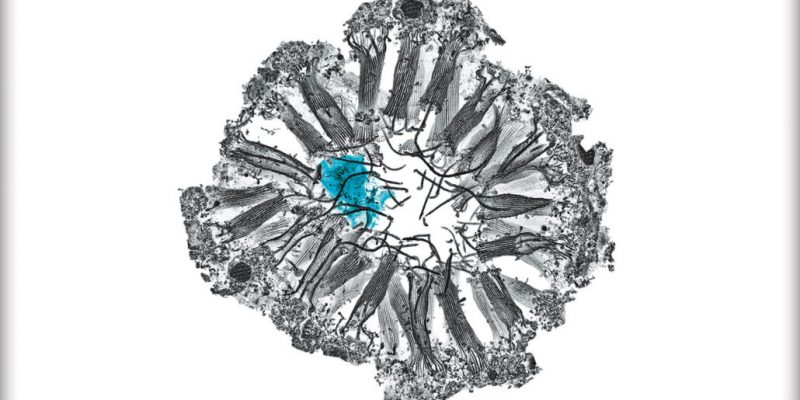
The good news is that vaccinated people aren’t unarmed against these mutated foes. The immune system launches a multipronged attack against invaders, so the response can handle small molecular tweaks to viruses, says Nina Luning Prak, an immunologist at the University of Pennsylvania. Dealing with variants “is what the immune system does.”
Vaccine-prompted antibodies still attack alpha and delta, though slightly less well than they tackle the original virus that emerged in Wuhan, China, two years ago. Antibodies also still recognize more immune-evasive variants such as beta, first identified in South Africa in May 2020, and gamma, identified in Brazil in November 2020. Although protection against infection dips against many of these variants, vaccinated people remain much less likely to be hospitalized compared with unvaccinated people.
Experts will continue to track how well the vaccines are doing, especially as new variants, like omicron, emerge. In late November, the World Health Organization designated the omicron variant as the latest variant of concern after researchers in South Africa and Botswana warned that it carries several worrisome mutations. Preliminary studies suggest that, so far, omicron is spreading fast in places including South Africa and the United Kingdom, and can reinfect people who have already recovered from an infection. The variant might be at least as transmissible as delta, though that’s still far from certain, according to a December 9 report from researchers with Public Health England, a U.K. health agency. How omicron may affect vaccine effectiveness is also unclear. Pfizer’s two-dose shot, for instance, may be about 30 percent effective at preventing symptoms from omicron infections while a booster could bring effectiveness back up to more than 70 percent, according to estimates from Public Health England. But those estimates are based on low case numbers and could change as omicron spreads.
“This is the first time in history that we’re basically monitoring virus mutations in real time,” says Müge Çevik, an infectious diseases physician and virologist at the University of St. Andrews in Scotland. “This is what the viruses do. It’s just that we’re seeing it because we’re looking for it.”
But it’s unlikely that any new variant will take us back to square one, Çevik says. Because of the immune system’s varied defenses, it will be difficult for a coronavirus variant to become completely resistant to vaccine-induced protection. The vaccines are giving our immune systems the tools to fight back. — Erin Garcia de Jesús
The shots are safe, with few serious side effects
With billions of doses distributed around the world, the shots have proved not only effective, but also remarkably safe, with few serious side effects.
“We have so much safety data on these vaccines,” says Kawsar Talaat, an infectious diseases physician at the Johns Hopkins Bloomberg School of Public Health. “I don’t know of any vaccines that have been scrutinized to the same extent.”
Commonly reported side effects include pain, redness or swelling at the spot of the shot, muscle aches, fatigue, fever, chills or a headache. These symptoms usually last only a day or two.
More rare and serious side effects have been noted. But none are unique to these shots; other vaccines — plus infectious diseases, including COVID-19 — also cause these complications.
One example is inflammation of the heart muscle, known as myocarditis, or of the sac around the heart, pericarditis. Current estimates are a bit squishy since existing studies have different populations and other variables (SN Online: 10/19/21). Two large studies in Israel estimated that the risk of myocarditis after an mRNA vaccine is about 4 of every 100,000 males and 0.23 to 0.46 of every 100,000 females, researchers reported in October in the New England Journal of Medicine. Yet members of Kaiser Permanente Southern California who had gotten mRNA vaccines developed myocarditis at a much lower rate: 5.8 cases for every 1 million second doses given, researchers reported, also in October, in JAMA Internal Medicine.
What all the studies have in common is that young males in their teens and 20s are at highest risk of developing the side effect, and that risk is highest after the second vaccine dose (SN Online: 6/23/21). But it’s still fairly rare, topping out at about 15 cases for every 100,000 vaccinated males ages 16 to 19, according to the larger of the two Israeli studies. Males in that age group are also at the highest risk of getting myocarditis and pericarditis from any cause, including from COVID-19.
Components of the mRNA vaccines may also cause allergic reactions, including potentially life-threatening anaphylaxis. The U.S. Centers for Disease Control and Prevention calculated that anaphylaxis happens at a rate of about 0.025 to 0.047 cases for every 10,000 vaccine doses given.
But a study of almost 65,000 health care system employees in Massachusetts suggests the rate may be as high as 2.47 per 10,000 vaccinations, researchers reported in March in JAMA. Still, that rate is low, and people with previous histories of anaphylaxis have gotten the shots without problem. Even people who developed anaphylaxis after a first shot were able to get fully vaccinated if the second dose was broken down into smaller doses (SN Online: 6/1/21).
The only side effect of the COVID-19 vaccines not seen with other vaccines is a rare combination of blood clots accompanied by low numbers of blood-clotting platelets. Called thrombosis with thrombocytopenia syndrome, or TTS, it’s most common among women younger than 50 who got the Johnson & Johnson vaccine or a similar vaccine made by AstraZeneca that’s used around the world (SN Online: 4/23/21).
About 5 to 6 TTS cases were reported for every 1 million doses of the J&J vaccine, the company reported to the U.S. Food and Drug Administration. The clots may result from antibodies triggering a person’s platelets to form clots (SN Online: 4/16/21). Such antibodies also cause blood clots in COVID-19 patients, and the risk of developing strokes or clots from the disease is much higher than with the vaccine, Talaat says. In one study, 42.8 of every 1 million COVID-19 patients developed one type of blood clot in the brain, and 392.3 per 1 million developed a type of abdominal blood clot, researchers reported in EClinicalMedicine in September.
“Your chances of getting any of these side effects, except for the sore arm, from an illness with COVID are much higher” than from the vaccines, Talaat says. — Tina Hesman Saey
Getting everyone vaccinated is … complicated
The quest to vaccinate as many people as quickly as possible this year faced two main challenges: getting the vaccine to people and convincing them to take it. Strategies employed so far — incentives, mandates and making shots accessible — have had varying levels of success.
“It’s an incredibly ambitious goal to try to get the large majority of the country and the globe vaccinated in a very short time period with a brand-new vaccine,” says psychologist Gretchen Chapman of Carnegie Mellon University in Pittsburgh, who researches vaccine acceptance. Usually “it takes a number of years before you get that kind of coverage.”
Globally, that’s sure to be the case due to a lack of access to vaccines, particularly in middle- and lower-income countries. The World Health Organization set a goal to have 40 percent of people in all countries vaccinated by year’s end. But dozens of countries, mostly in Africa and parts of Asia, are likely to fall far short of that goal.
In contrast, the United States and other wealthy countries got their hands on more than enough doses. Here, the push to vaccinate started out with a scramble to reserve scarce appointments for a free shot at limited vaccination sites. But by late spring, eligible people could pop into their pharmacy or grocery store. Some workplaces offered vaccines on-site. For underserved communities that may have a harder time accessing such vaccines, more targeted approaches where shots are delivered by trusted sources at community events proved they could boost vaccination numbers (SN Online: 6/18/21).
Simply making the shot easy to get has driven much of the progress made so far, Chapman says. But getting people who are less enthusiastic has proved more challenging. Many governments and companies have tried to prod people, initially with incentives, later with mandates.
Free doughnuts, direct cash payments and entry into million-dollar lottery jackpots were among the many perks rolled out. Before the pandemic, such incentives had been shown to prompt some people to get vaccines, says Harsha Thirumurthy, a behavioral economist at the University of Pennsylvania. This time, those incentives made little difference nationwide, Thirumurthy and his colleagues reported in September in a preliminary study posted to SSRN, a social sciences preprint website. “It’s possible they moved the needle 1 or 2 percentage points, but we’ve ruled out that they had a large effect,” he says. Some studies of incentives offered by individual states have found a marginal benefit.
“People who are worried about side effects or safety are going to be more difficult to reach,” says Melanie Kornides, an epidemiologist at the University of Pennsylvania. And with vaccination status tangled up in personal identity, “you’re just not going to influence lots of people with a mass communication campaign right now; it’s really about individual conversations,” she says, preferably with someone trusted.
“Or,” she adds, “they’re going to respond to mandates.” Historically, sticks such as being fired from a job or barred from school are the most effective way of boosting vaccination rates, Kornides says. For example, hospitals that require flu shots for workers tend to have higher vaccination rates than those that don’t. For decades, mandates in schools have helped push vaccination rates up for diseases like measles and chickenpox, she says.
As COVID-19 mandates went into effect in the fall, news headlines often focused on protests and refusals. Yet early anecdotal evidence suggests some mandates have helped. For instance, after New York City public schools announced a vaccine requirement in late August for its roughly 150,000 employees, nearly 96 percent had received at least one shot by early November. Still, about 8,000 employees opted not to get vaccinated and were placed on unpaid leave, the New York Times reported.
Many people remain vehemently opposed to the vaccines, in part because of rampant misinformation that can spread quickly online. Whether more mandates, from the government or private companies, and targeted outreach will convince them remains to be seen. — Jonathan Lambert
Vaccines can’t single-handedly end the pandemic
One year in, it’s clear that vaccination is one of the best tools we have to control COVID-19. But it’s also clear vaccines alone can’t end the pandemic.
While the jabs do a pretty good job preventing infections, that protection wanes over time (SN Online: 3/30/21). Still, the vaccines have “worked spectacularly well” at protecting most people from severe disease, says Luning Prak, the University of Pennsylvania immunologist. And as more people around the world get vaccinated, fewer people will die, even if they do fall ill with COVID-19.
“We have to make a distinction between the superficial infections you can get — [like a] runny nose — versus the lower respiratory tract stuff that can kill you,” such as inflammation in the lungs that causes low oxygen levels, Luning Prak says. Preventing severe disease is the fundamental target that most vaccines, including the flu shot, hit, she notes. Stopping infection entirely “was never a realistic goal.”
Because vaccines aren’t an impenetrable barrier against the virus, we’ll still need to rely on other tactics to help control spread amid the pandemic. “Vaccines are not the sole tool in our toolbox,” says Saad Omer, an epidemiologist at Yale University. “They should be used with other things,” such as masks to help block exposure and COVID-19 tests to help people know when they should stay home.
For now, it’s crucial to have such layered protection, Omer says. “But in the long run, I think vaccines provide a way to get back to at least a new normal.” With vaccines, people can gather at school, concerts or weddings with less fear of a large outbreak.
Eventually the pandemic will end, though when is still anyone’s guess. But the end certainly won’t mean that COVID-19 has disappeared.
Many experts agree that the coronavirus will most likely remain with us for the foreseeable future, sparking outbreaks in places where there are pockets of susceptible people. Susceptibility can come in many forms: Young children who have never encountered the virus before and can’t yet get vaccinated, people who choose not to get the vaccine and people whose immunity has waned after an infection or vaccination. Or the virus may evolve in ways that help it evade the immune system.
The pandemic’s end may still feel out of reach, with the high hopes from the beginning of 2021 a distant memory. Still, hints of normalcy have returned: Kids are back in school, restaurants and stores are open and people are traveling more.
Vaccines have proved to be an invaluable tool to reduce the death and destruction that the coronavirus can leave in its wake. — Erin Garcia de Jesús