Health official calls on neuroscience to fight mental illness
SAN DIEGO — Society’s record for protecting public health has been pretty good in the developed world, not so much in developing countries. That disparity has long been recognized.
But there’s another disparity in society’s approach to public health — the divide between attention to traditional diseases and the resources devoted to mental disorders.
“When it comes to mental health, all countries are developing countries,” says Shekhar Saxena, director of the World Health Organization’s department of Mental Health and Substance Abuse. Despite a breadth of scope and depth of impact exceeding that of many more highly publicized diseases, mental illness has long been regarded as a second-class medical concern. And modern medicine’s success at diagnosing, treating and curing many other diseases has not been duplicated for major mental disorders.
Saxena thinks that neuroscience research can help. He sees an opportunity for progress through increased interdisciplinary collaboration between neuroscience and mental health researchers.
“The collaboration seems to be improving, but much more is needed and not only in a few countries, but all countries,” he said November 12 at the annual meeting of the Society for Neuroscience.
By almost any measure, mental health disorders impose an enormous societal burden. Worldwide, direct and indirect costs of mental disorders exceed $2.5 trillion yearly, Saxena said — projected to reach $6 trillion by 2030. Mental illnesses also disable and kill in large numbers: Global suicides per year total over 800,000. “Indeed, it is a hidden epidemic,” Saxena said. That’s more deaths than from breast cancer and probably more from malaria, according to a new comprehensive analysis of global mortality.
Mental illnesses encompass a wide range of disorders, from autism and Alzheimer’s disease to substance abuse and schizophrenia. Saxena acknowledged that there have been advances in the scientific understanding of these diseases, but not nearly enough. No easily used diagnostic test is available for most of them. And no new class of drugs for treating major mental disorders has appeared in the last 20 years, with the possible exception of dementia.
“We need increased investment in research, increased public, private and philanthropic investments,” Saxena said. “We need increased connection of research with public health gains.”
He called on the community of neuroscientists to establish a “grand challenge” to researchers to address these concerns.
“There have been many grand challenges in neurosciences — perhaps we need one for finding out mental health interventions,” he said.
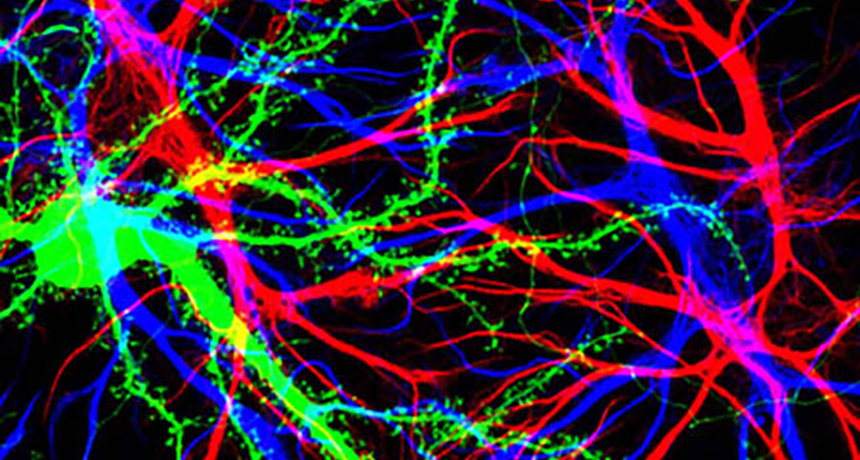
Many neuroscientists are, of course, aware of the important link between their research and mental health. Some progress is being made. One promising avenue of work focuses on synapses, the junctures through which nerve cells in the brain communicate. Typically synapses form where axons, the long neuronal extensions that transmit signals, connect with dendrites, the neurons’ message-receiving branches. Most of the axon-dendrite connections occur at small growths called dendritic spines that protrude from the dendrite surface.
Several sessions at the neuroscience meeting described new work showing ways in which dendritic spines may be involved in mental disorders. One session focused on the protein actin, a prime structural component of the spines.
Actin activity depends on a complicated chain of chemical reactions inside a cell. In mice, blocking a key link in that chain reduces the number of spines in the front part of the brain, Scott Soderling of Duke University School of Medicine reported. Those mice then exhibited symptoms reminiscent of schizophrenia in people.
It seems that losing spines in the frontal cortex alters nerve cell connections there; with spine shortages, some axons link directly to the dendrite shaft. Bypassing spines, which play a filtering role, can intensify signals sent to the ventral tegmental area, which in turn may send signals that increase production of the chemical messenger dopamine in another brain region, the striatum. “We think that this is actually what is driving the elevated dopamine levels” in disorders such as schizophrenia, Soderling said.
Some antipsychotic drugs (known as neuroleptics) for treating schizophrenia work by blocking sites of dopamine action in the striatum. But such drugs do nothing about the loss of spines that initiated the problem.
“These neuroleptics largely treat these symptoms, but they’re not a cure,” Soderling said. “We think that this is good evidence … for the idea that these drugs are treating a downstream consequence of a primary insult that’s occurring elsewhere in the brain.”
This insight from neuroscience — that antipsychotics treat downstream symptoms, not the problem at its source — may help the search for better treatments.
Soderling suggests that many other mental disorders may have their roots in problems with actin in dendritic spines. Another speaker at the neuroscience meeting, Haruo Kasai of the University of Tokyo, emphasized how fluctuations in the numbers of spines, related to actin activity, could play a role in autism.
Such results from neuroscience should be of great value to fighting mental disorders. But science alone won’t enable the discovery of effective treatments without a broader scope of scientific investigation of mental illness as a global problem. Too much of research to date focuses on too small a portion of the worldwide population. As Saxena noted, more than 90 percent of scientific studies on mental illness are from — and about — high-income countries.
“We are ignoring a very large number of people living in this world,” he said. “And this can be, and is, a real impediment to science. If we don’t know what is happening in the brains of the majority of the people living in this world, can we really advance science in the best possible manner? Can we still say that we know the human brain? And at least my answer would be: No.”